Abstract

Introduction:
Primary cutaneous T cell lymphomas (PCTCL) including Mycosis fungoides (MF) and Sézary syndrome (SS) account for 75% of primary cutaneous lymphomas. The 5-year survival is 18-40% in patients with advanced-stage PCTCL. Management strategies and prognosis of PCTCL depend on the disease stage (affected body surface area, blood, visceral and nodal involvement). Allogeneic hematopoietic cell transplantation (allo-HCT) can be used to treat advanced stages in young adults who are otherwise in good health. However, post-transplant relapse is still an issue with no clear guidelines regarding its management. Here we describe the largest study investigating donor lymphocyte infusions (DLI) in patients who relapsed after allo-HCT for PCTCL.
Patients and methods:
We conducted an observational, retrospective, French multicenter study. Between January the 1st 2000 and December the 31st 2017, all patients who underwent an allo-HCT for PCTCL regardless of the subtype and who received DLI for a post-transplant relapse were included. Data were collected using the ProMISE database. As needed, centers were asked to provide additional data.
Statistical analyses were carried out by the Lille University Hospital (CHRU Lille) Biostatistics Methodology Unit and were performed using SAS software (SAS Institute version 9.4).
Results:
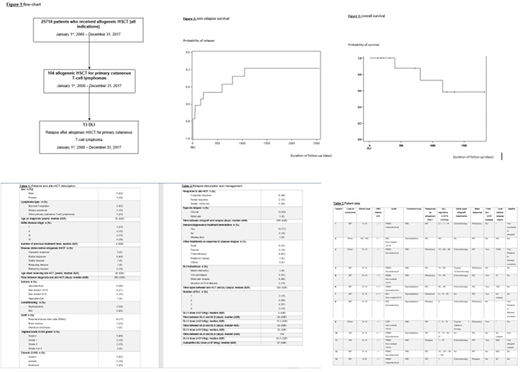
All 13 patients who received DLI after allo-HCT for a PCTCL in France were enrolled in the study (Figure 1). Mean duration of follow-up was 718 days. See table 1 for study population characteristics. Four patients (30%) presented acute graft versus host disease (GVHD) following allo-HCT, of which no incidences were superior to grade 2. Those four patients relapsed at day 342, 463, 499 and 659 after allo-HCT. Five patients (38%) presented chronic GVHD of which three had an extensive presentation. Those three patients relapsed at day 1082, 1568 and 1861.
Table 2 details relapses and relapse management in our cohort. Table 3 shows parameters relative to allo-HCT, post-therapeutic management, and follow-up.
Objective response rates to DLI was 62% (n=8). Five patients (38%) showed complete response and three patients exhibited partial response (32%). Five patients (38%) did not respond to DLI.
The median best response duration to DLI was 181 days. Six out of the eight patients who responded to DLI relapsed (75%); the median time before the relapse after DLI was of 405 days. The two patients who have received DLI and did not relapse on January the 1st 2018 had 321 and 1350 days follow-up. Progression-free survival (PFS) was 46% at 1 year and 19% at 5 years (Figure 2). Overall survival rates were 100% at 1 year and 59% at 5 years (Figure 3).
Six patients (46%) presented GVHD after DLI of which three cases were chronic GVHD. Two of them was an extensive presentation. One patient had received an allo-HCT from a female donor. One patient received bone marrow transplant carrying a 9/10 mismatch. All other patients received peripheral blood stem cell (PBSC) transplantation; two of them received a geno-identical stem cell transplantation from sibling donors and three patients received non-sibling donor HSCT with a 10/10 mismatch. Only three patients received DLI following SFGM-TC guidelines.
Four patients died before January the 1st 2018 in our cohort. One patient died because of direct complications of the HSCT and related treatments. Two patients died because of a disease relapse. One patient died from unrelated cause (severe pulmonary).
Conclusion:
With a 5-year survival rate of 59% from the date of post-transplant relapse, DLI appears to be an effective treatment in cases of patient relapse after allo-HCT for PCTCL. DLI should be considered in the management of post-transplant relapse whenever possible. To our best knowledge, this is the largest study cohort investigating DLI in the post-transplant setting
Bagot:Takeda: Membership on an entity's Board of Directors or advisory committees; Actelion: Membership on an entity's Board of Directors or advisory committees; Kyowa Kirin: Membership on an entity's Board of Directors or advisory committees; Innate Pharma: Consultancy, Equity Ownership, Membership on an entity's Board of Directors or advisory committees. Peffault De Latour:Amgen Inc.: Research Funding; Alexion Pharmaceuticals, Inc.: Consultancy, Honoraria, Research Funding; Novartis: Consultancy, Honoraria, Research Funding; Pfizer Inc.: Consultancy, Honoraria, Research Funding.
Author notes
Asterisk with author names denotes non-ASH members.

This icon denotes a clinically relevant abstract

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal